However, the city faces ongoing challenges, including dilapidated infrastructure, human resources issues, and a lack of effective incentive policies.
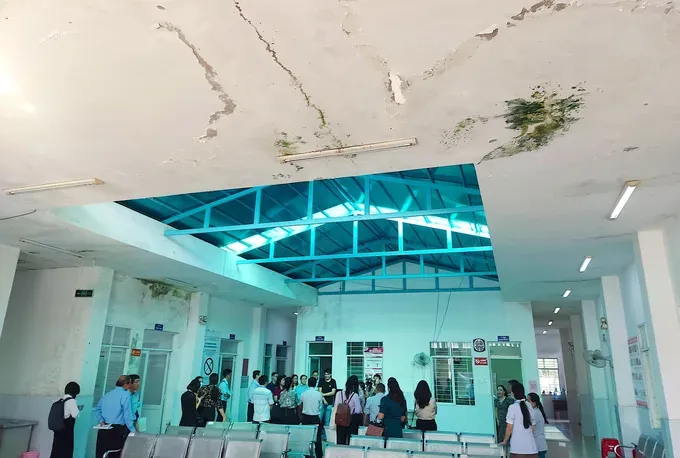
While Ho Chi Minh City has invested hundreds of billions of Vietnamese dong to upgrade 55 of its 464 health stations and medical outposts, numerous facilities remain in a state of disrepair. Many health stations, medical outposts, and regional health centers urgently require reconstruction.
Dr. Le Thanh Quyet, Deputy Director of the Go Vap District Medical Center, reported that nine of the fourteen health stations and medical outposts in his district need significant renovation or repair. The Go Vap District Medical Center, nearly 50 years old, has also seriously deteriorated.
Deputy Director Le Thanh Quyet stated that in 2023, the city had a plan to renovate, repair, and rebuild local health stations, but so far none of the nine stations in the district have seen any projects implemented.
The Ho Chi Minh City Management Board for Civil and Industrial Construction Projects, the investor for the projects, cited both internal and external factors for the delays in renovating 146 health stations. The Board noted that while some local authorities have been effective in their planning, others have not coordinated closely, causing delays in project approval. Consequently, the Board has proposed to the HCMC People's Committee that these projects be temporarily suspended and deferred to the 2026–2030 period.
Beyond health stations, the city is also facing delays in new hospital construction projects. For instance, Khanh Hoi Hospital, after decades of operation, now suffers from warped floor tiles, leaking walls, substandard patient rooms, and outdated medical equipment.
Likewise, Phu Nhuan Hospital faces severe deterioration and overcrowding. Despite its limited space, much of the hospital's courtyard has to be used as a parking lot to accommodate the 1,500–2,000 patients who visit daily for examination and treatment.
In addition, the city's healthcare sector continues to face a shortage of personnel, particularly at the primary healthcare level, due to incentive policies that fail to attract and retain medical staff. Leaders of several regional hospitals noted that current allowances for healthcare workers remain inadequate; for example, the 24-hour on-call allowance has stayed at VND90,000 (US$3.4) per shift for the past 14 years, even though the base salary has been adjusted upward eight times and is now at a coefficient of 2.34.
Other allowances for on-call duty, surgeries, and procedures have also not been adjusted accordingly.
Investing in the front line: Strengthening primary healthcare
Health experts assert that shifts in disease patterns, including the rise of non-communicable diseases and an aging population, necessitate higher-quality primary healthcare services. To meet this demand, it is crucial to resolve bottlenecks in infrastructure, human resources, and the digitalization of medical records.
Assoc. Prof. Phung Nguyen The Nguyen, Head of the Faculty of Medicine at the University of Medicine and Pharmacy in Ho Chi Minh City, emphasized that the city’s primary healthcare system must shift its focus from passive treatment to proactive health protection. A key component of this shift is ensuring adequate and properly allocated personnel.
Dr. Nguyen proposed that each health station be staffed with a family doctor, community nurse, pharmacist, and rehabilitation technician. He stressed that personnel allocation should be based on local needs and disease prevalence, not a uniform distribution. He also highlighted the need for staff retraining to focus on prevention rather than just treatment. This retraining should cover family medicine, chronic disease management, infection prevention, and continuous care across the life cycle.
He stated that the role of primary healthcare staff should evolve from treating existing illnesses to actively preserving community health. According to Dr. Nguyen, a crucial preventative measure is to expand adult vaccination programs to include diseases such as influenza, pneumococcal disease, and hepatitis, in addition to maintaining full immunization coverage for children.
At the same time, early screening programs for cardiovascular disease, diabetes, and cancer should be implemented at the grassroots level to ease the burden on higher-tier hospitals, emphasized Assoc. Prof. Phung Nguyen The Nguyen.
Dr. Tran Van Khanh, Director of Le Van Thinh Hospital, explained that the hospital has recently supported primary healthcare by establishing satellite polyclinics at several health stations in An Khanh and Binh Trung wards. As a result, the effectiveness of medical services at the local level has improved significantly, with an average of 300–500 patient visits per day.
According to the Ho Chi Minh City Department of Health, the city currently has 38 medical centers, 168 commune health stations, and 296 healthcare points. However, the city healthcare system employs only about 1,800 medical staff, averaging 5–10 personnel per station. With a population exceeding 14 million, each healthcare worker is responsible for caring for 6,000–6,500 residents. This workload is excessively high, leading to a decline in the quality of healthcare services.